
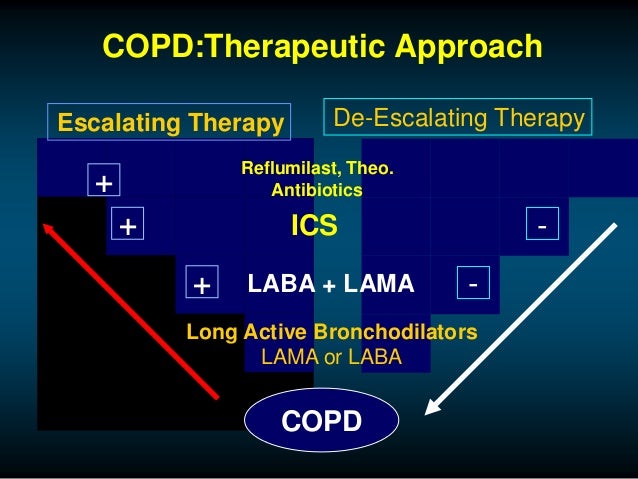
Dual therapy also showed a significantly longer time to first exacerbation compared with LABA in the GOLD III/IV group. In the GOLD III/IV group, dual therapy was significantly more effective in improving FEV 1, reducing SGRQ scores, and achieving a higher proportion of SGRQ responders compared with either LABA or LAMA. ResultsĪ total of 14,449 group B patients from 12 studies were divided into GOLD III/IV (n = 8043) or GOLD I/II group (n = 6406). George’s Respiratory Questionnaire (SGRQ) score, the proportion of SGRQ responders, time to first exacerbation, and risk of adverse events. We evaluated the efficacy of dual versus monotherapy (long-acting beta-2 agonist or long-acting muscarinic antagonist ) between these two groups in the following outcomes: changes in trough FEV 1, the St. Study patients were classified into two groups based on the FEV 1 of 50% of the predicted value (GOLD I/II versus GOLD III/IV).
This was a patient-level pooled analysis of phase-3 randomized controlled trials involving dual bronchodilators. We evaluated if a lower forced expiratory volume in 1 s (FEV 1) identifies a population more likely to benefit from dual therapy than monotherapy among group B COPD patients in whom Global initiative for Chronic Obstructive Pulmonary Disease (GOLD) recommends monotherapy as initial treatment. Which patients should receive dual therapy as initial treatment for chronic obstructive pulmonary disease (COPD) is only loosely defined.


 0 kommentar(er)
0 kommentar(er)
